Topic One: Peripheral Neuropathy
The IWGDF (2019) defines diabetes-related peripheral neuropathy as “The presence of signs or symptoms of peripheral nerve dysfunction in people with diabetes after exclusion of other causes”.
Nerve dysfunction affects three different types of nerves in the lower legs and feet:
- Sensory
- Motor
- Autonomic
These are three types of neuropathies which can occur in isolation or together.
Sensory neuropathy
Approximately 45–60% of all DFUs are due to sensory neuropathy (Frykberg et al., 2006). The loss of sensation associated with sensory neuropathy puts the patient at risk of mechanical, chemical and thermal trauma. There are several tests that can be used to determine the degree of sensory loss.
Monofilament Test: This is the most frequently used screening tool to determine the presence of neuropathy in patients with diabetes (Boulton et al., 2008; NICE, 2016). A 10g monofilament is applied to specific areas of the foot perpendicularly until the monofilament buckles and holds for two seconds each time with the patient’s eyes closed and answering “yes” each time they feel it. A positive result is the inability to feel the monofilament when it is pressed against the foot with enough force to bend it (Clayton & Elasy, 2009; International Diabetes Federation, 2017).
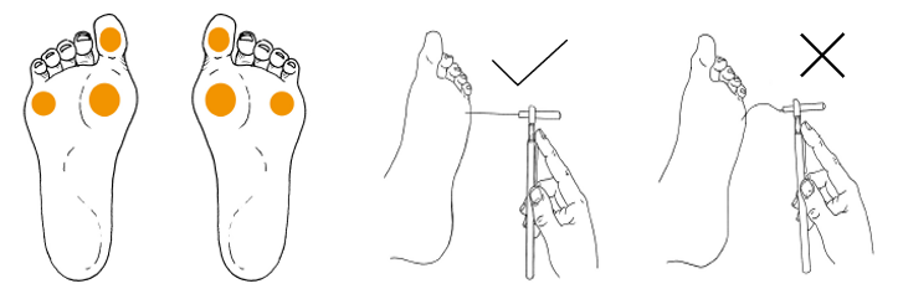
The monofilament sites and method of use.
Neurotip: A small (single use) device with a blunt tip at one end and a sharp tip at the other. The ends are randomly applied to designated areas on the sole of the foot, to ascertain if the patient has the ability to distinguish between sharp and blunt sensations.
Vibration testing: Place the vibrating fork (128HZ) on the patient’s big toe (distal hallux) joint and check if they can feel vibration (demonstrated prior to testing on a bony prominence on the hand). Neuropathy is demonstrated by an inability to sense degrees of strength and the pathway of vibrations.
A biothesiometer or neurothesiometer can also be used for assessing the perception of vibration. (International Diabetes Federation, 2017; IWGDF, 2019)
Light touch test: Also called the Ipswich Touch test, it can be used to screen for loss of protective sensation when the 10-gram monofilament or 128 HZ tuning fork is not available. The patient closes their eyes, and the examiner lightly, sequentially touches with the tip of their index finger the tips of the first, third, and fifth toes of both feet for 1–2 seconds. Its accuracy on use, in predicting foot ulcers has not been established (IWGDF, 2019).
Temperature sensation test: This can be done simply with the application of the cold metal from a tuning fork to nominated anatomical areas on the sole of the foot or using a device such as a Tip Them, which creates differential heat conductance between tips. This informs the practitioner if the person has the ability to identify cold. Caution is to be taken with the application of heat to the limb, especially if neuropathy is suspected as it may cause thermal trauma.
Motor neuropathy
Impairment of the nerves controlling muscles causes muscular atrophy in the foot. This causes two problems:
- Muscle atrophy in the toes, which causes claw toes. The tips of the toes can then rub against the shoes leading to ulceration.
- Foot deformities (e.g. crooked toes or hammer toes) develop as the person’s gait changes. This can then cause repetitive stresses on certain areas of the foot (often the metatarsal head). Callus formation is the first indicator for repetitive stress, this will progress to ulceration if preventative measures are not taken (Wounds International, 2013).
Autonomic neuropathy
Diabetic patients with autonomic neuropathy will experience a lack of sweating in the feet, which can extend up to the knees and can be patchy in distribution.
Autonomic neuropathy is typically associated with dry skin, which can result in fissures, cracking and calluses. Another feature is bounding pulses, which is often misinterpreted as indicating good circulation. It can also cause distended veins.
Typical signs of Neuropathy are the loss of the sensation to light touch, pain and temperature. Lack of the sensation of pain significantly increases the risk of unnoticed injury or trauma that can lead to tissue breakdown and foot ulceration.
| TYPE OF NEUROPATHY | CLINICAL SIGNS | CLINICAL IMPLICATIONS |
|---|---|---|
| Sensory neuropathy | Loss of sensation to light touch, pain and temperature. | Loss of pain significantly increases the risk of unnoticed injury or trauma that can lead to tissue breakdown and foot ulceration. |
| Motor neuropathy | Poor nerve supply to the muscles in the leg and the foot can cause foot deformities. | Foot deformities cause the foot to function abnormally. This can result in high areas of pressure on the foot that can lead to foot ulceration. |
| Autonomic neuropathy | Absence of sweating (anhidrosis) in the foot can cause dry skin. | Anhidrosis can lead to callus formation and skin fissures (cracks in the skin), which can increase the risk of infection and ulceration in the diabetic foot. |
Signs and symptoms of peripheral neuropathy (McIntosh & Halford, 2014)