Topic Two: Neuroischaemia
Neuroischaemia is the combined effect of diabetic neuropathy and ischaemia, whereby macrovascular disease and, in some instances, microvascular dysfunction impair perfusion in a diabetic foot (Wounds International, 2013). Ischaemia results from atherosclerosis of the arteries in the leg. Claudication is often absent due to coexisting neuropathy.
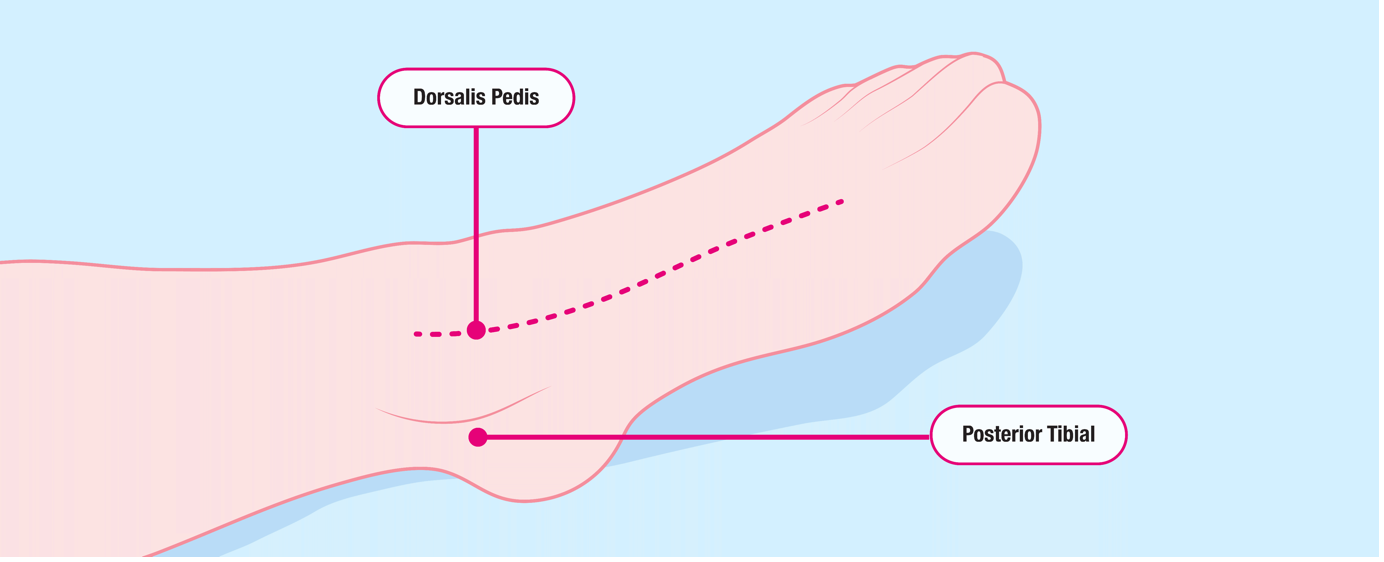
One of the most common assessment techniques to detect ischaemia is the palpation of foot pulses.
Dorsalis pedis pulse – lateral to the extensor hallucislongus tendon on the dorsum of the foot.
Posterior tibial pulse – above and behind the medial malleolus.
Weak or absent pulses point to occlusion, stenosis or calcification proximal to the abnormal findings. However, the presence of pedal pulses does not always indicate adequate circulation nor exclude peripheral arterial disease (PAD), as collateral blood flow may be enough to maintain a palpable pulse.
Palpation of peripheral pulses should be part of the physical examination (but not the only component), including the assessment of the dorsalis pedis and posterior tibial pulses.
It is important to note that the assessment of pulses is a learned skill and has a high degree of inter-observer variability. The absence of both pedal pulses can strongly suggest peripheral vascular disease affecting the foot (Wounds International, 2013).
There are other methods that can be used to establish the degree of PAD and ischaemic risk such as those listed below.
Toe Brachial Pressure Index – Non-invasive way of determining arterial perfusion in feet and toes, similar to ABPI. To determine the TBPI, a Doppler device and a sphygmomanometer are used to measure systolic pressure in the arm and the great toe. The readings are used to calculate the results as follows:
TBPI =
Toe systolic pressure
Brachial systolic pressure
Transcutaneous oxygen (tcpO2) – Electrodes measure the partial pressure of oxygen through the skin. Assesses the nutritive skin capillary circulation and can be used to determine the severity and clinical progression of PAD
ABPI, duplex scanning and arteriography may also be utilised. (Please refer to Module 5.1: Lower Limb Ulcers)
The ischaemic foot may display several classic signs:
- It may have thin shiny skin that lacks hair.
- There may be atrophy of the subcutaneous tissue. If the skin appears dusky red or cyanotic blue this may be due to impaired perfusion, causing stagnation of blood in the dilated arterioles.
- In acute ischaemia, the foot is often cold and pale or mottled.
- A patient with acute limb ischaemia characterised by the six ‘Ps’ - pulselessness, pain, pallor (mottled colour), perishing cold, paresthesia and paralysis.
Any patient exhibiting these signs is a potential medical emergency and needs to be managed in a timely and effective way (Wounds International, 2013).