PRESSURE INJURIES
Please note:
The term pressure injuries/ulcers is interchangeable, and the term used will depend on the country. For this module, it will be referred to as pressure injuries/ulcers or PI/PU.
Definition & Prevalence
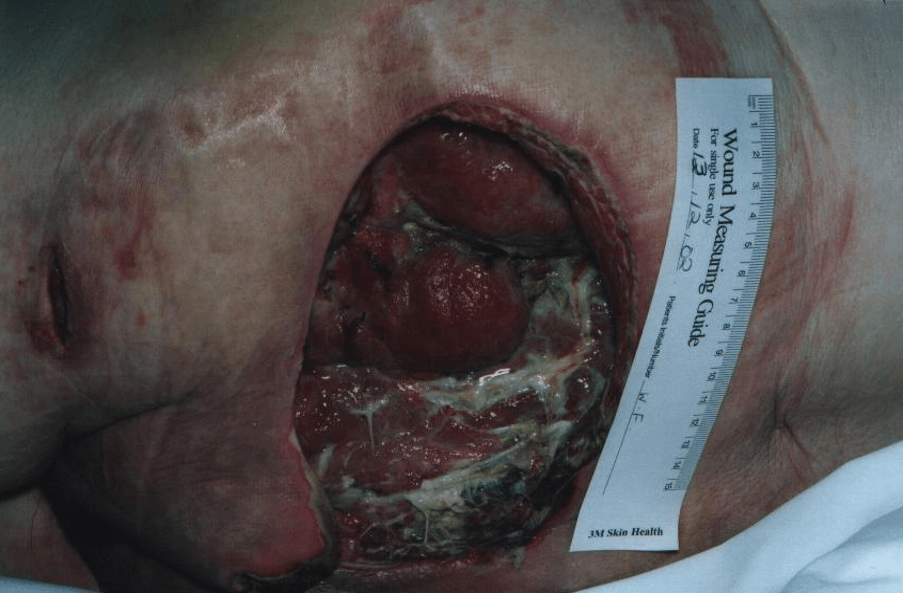
‘Localised damage to the skin and underlying soft tissue usually over a bony prominence or related to a medical or other device. The injury can present as intact (or unbrocken) skin or an open wound, and may be painful. The injury occurs because of intense and/or prolonged pressure or pressure in combination with shear. The tolerance of soft tissue for pressure and shear may also be affected by microclimate, nutrition, perfusion, comorbidities, and condition of the soft tissue’. EUPAP, 2019
Pressure injuries are a frequently occurring health problem throughout the world. They are a painful, costly, and often preventable complication of which many individuals are at risk. EUPAP, 2019
Globally, pressure injury prevalence in healthcare settings ranges from 0.1% to 72.5%, with variations observed between different geographic and clinical settings. In general, within acute care, there is a gradual and continual decline in pressure injury prevalence over the past two decades, driven primarily by increasing international health policy focus on pressure injury prevention. EUPAP, 2019
Pressure injuries also represent a major burden of illness and reduced quality of life for patients and their care givers. There is also an increase in morbidity and mortality associated with pressure injury development, alongside longer stay in hospital, readmission rates, and financial costs.
The impact of living with the burden of a pressure injury is the same as with a chronic wound, including pain, discomfort, stress, anxiety, and depression. Correspondingly, declines in autonomy, security, mental health, general well-being, and social functioning. Those individuals at risk or having pressure injuries identify pain as one of their most significant concerns. EUPAP, 2019
A pressure injury can occur due to the forces of a patient’s body weight, because of externally exerted forces such as those applied by a medical device or other object, or by a combination of these. The injury can present as intact (or unbroken) skin or an open wound and may be painful.
The tissue damage occurs because of intense and/or prolonged exposure to the following:
Pressure
When a force is applied perpendicular (at right angles) to the surface of the skin, pressure occurs on the skin and subcutaneous tissues. The pressure compresses the tissues and can distort or deform skin and soft tissues such as subcutaneous fat and muscle. Deformation of soft tissues is greater when pressure is applied over a bony prominence.
Friction and shear
Friction, shear and pressure are interlinked. Friction is the force that occurs when two objects that are touching are encouraged to move relative to each other.
An example of this is when a patient slips down the bed due to gravity, friction is present between the skin and a support surface. Friction cannot occur without some element of pressure. The amount of friction produced will depend on the interaction, how easily the skin and support surface move across each other, and how much pressure is applied.
Shear may result from the application of a tangential force, that is a force that is parallel to the surface of the skin. When there is a high level of friction between the skin and a support surface, and a tangential force occurs, the skin will tend to stay in place against the support surface while the layers of underlying tissues are deformed as they move with the patient.
Microclimate
This usually relates to temperature and moisture at the skin–support surface interface. The concept was developed when increased tissue temperature and skin moisture were recognised as risk factors for pressure ulcer/injury (PU/PI) occurrence.
Increased skin temperature has several metabolic and physical effects that can amplify the risk of skin damage from external influences.
High moisture levels at the skin–support surface interface can have various causes, such as perspiration, incontinence, and wound/fistula drainage. They may contribute to the development of PU/PIs by weakening and increasing the amount of friction between the skin and a support surface. EUPAP, 2019; WUWHS, 2016
Most pressure ulcers/injuries develop when soft tissue is compressed between a bony prominence (e.g. the sacrum) and an external surface (e.g. mattress or chair). There are intrinsic and extrinsic factors that will increase an individual’s risk of pressure ulcer/injury development.
When pressure is applied, either with great force for a short time or with less force over a longer time, it disrupts the blood supply to the surrounding tissues. This deprives that area of oxygen and nutrients, leading to local ischaemia and eventually cell death. EPUAP, 2019