LEG ULCER PATHWAY
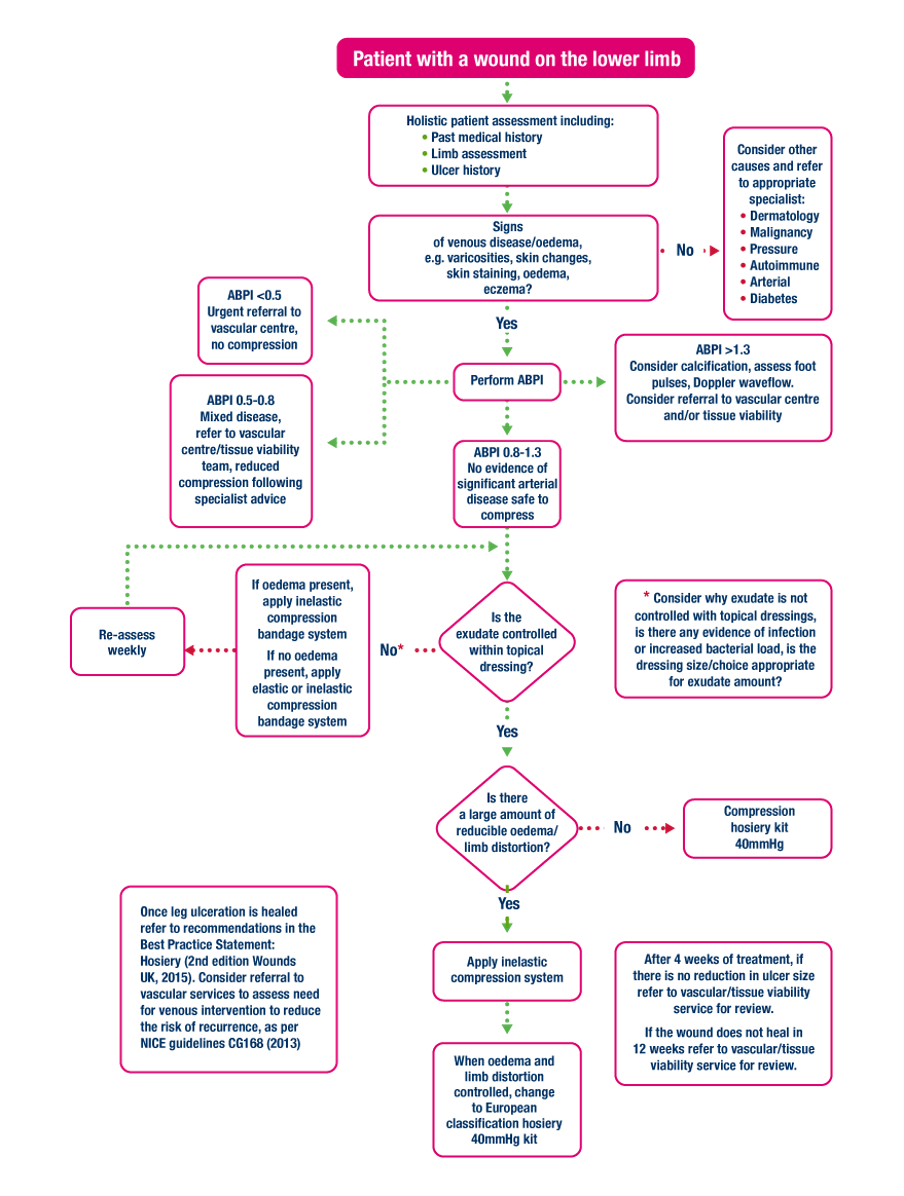
Adapted from Atkins & Tickle, 2016
ELEVATION
In addition to compression bandaging (if appropriate), advise the person to elevate their legs (above hip level) for 30 minutes, three to four times a day, and consider placing pillows under their feet and legs while sleeping. Bed rest and elevation may reduce oedema of the ankle and leg before compression bandages are applied (NICE, 2015).
MOBILITY
A patient mobilising optimises compression therapy. Encourage patients to be as mobile as possible, dependant on the individual’s capability. Walking regularly, exercising the legs - moving feet up and down, rotating the ankles. Try to avoid sitting still with feet pointing downwards. When sitting or lying down, elevate leg, ideally with toes being level with the heart (Wounds UK, 2015).
SKIN CARE
Skin care is a very important factor in the management of venous leg ulcers. It must take the following into consideration; eczema; scaling; allergies and wound infection (Dealey, 2005).
NUTRITIONAL SUPPORT
Maintaining a healthy and balanced diet and upholding an appropriate weight can assist in reducing the risks of developing a VLU. It also encourages the healing process in patients with existing wounds.
EDUCATION AND INFORMATION
The patient, where possible, should always be informed at all stages of their treatment. The views of the patient need to be considered and discussed, looking at their expectations and choices.
Patient involvement and engagement are key to being in agreement with the treatment and to accomplish a positive outcome (Wounds UK, 2016).
The patient and/or caregivers should be educated in order to be observant for any signs that they need to contact their clinician, e.g. trauma, changes to the lower leg, oedema, or concerns about a potential DVT (Wounds UK, 2016).
WOUND MANAGEMENT
After a thorough wound assessment, the aim is to heal the ulceration. There are several wound dressings that can aid healing, improve comfort, control exudate and are needed to prevent a bandage or compression hosiery from adhering to the wound (SIGN, 2010).
Before applying a dressing and, or compression, good wound hygiene should be undertaken. Wound bed cleansing and debridement, periwound and limb skin cleaning. Emollients can be used to help moisturise the surrounding skin as appropriate and required (NWCSP, 2020).
Compression therapy is the gold standard for leg ulcer treatment. However, NICE (2015) recommend a simple low adherent dressing, which may be all that is required. Alternative dressings may be considered to help with pain (hydrocolloid), heavy exudate (alginate, gelling fibres), or slough (dry, hydrogels). The choice of a wound management product must be based on a full patient and wound assessment.
At each dressing change, wound hygiene should continue, and if using compression therapy, a review of any reduction in ankle circumference observed and, if necessary, the type of compression reviewed (NWCSP, 2020).
Patients with venous leg ulcers must be reviewed at regular intervals to ensure that the current treatment regimen is still appropriate.
The National Wound Care Strategy Programme (UK, 2020) recommend that after initial treatment and assessment, the person and the wound should be reassessed at least every four weeks. Those who are showing no significant progress to wound healing or are showing any signs of deterioration should be escalated to the appropriate specialist service.
Where appropriate and possible, self-care should be encouraged and supported by the multidisciplinary team.
Once the venous ulcer has healed, it is essential that patients follow simple advice aimed at preventing the recurrence of the ulcer. This includes wearing compression stockings, skin care, leg elevation, calf exercises, and adopting a suitable diet (Grey et al., 2006; Wounds UK, 2016).