Pathophysiology of Venous Leg Ulceration
Venous leg ulceration is characterised by:
- Valves within the leg veins become damaged and are less able or completely unable to prevent back flow.
- The calf muscle pump may not be strong enough to push the blood upwards.
- Venous blood volume increases in the lower leg veins, which results in the pooling of blood.
- The vein walls stretch and allow fluid, including proteins and red cells, to leak into the tissues.
- The cells in the tissues become filled with fluid and they may swell and leak.
- The lymphatic system is unable to cope with the extra volume of fluid (lymphoedema).
- Venous congestion and hypertension mean that the nutrients do not get to the tissue and skin. This results in dry skin and often varicose eczema.
- Fluid in the leg is at risk of infection (cellulitis), and the skin and tissue are at risk of trauma.
(Anderson, 2006)
Poor valve performance can be caused by:
- Congenital or familial defect/disorder
- Damage from a previous deep vein thrombosis (DVT)
- Surgery
- Pregnancy
- Varicose veins
- Injury
- Mechanical defect due to a higher obstruction to venous return
(Newton, 2010)
Causes of calf muscle pump failure:
- Paralysis
- Immobility
- Fixed ankle joint
- Regular ‘chair sleeping’ combined with poor mobility canal so significantly impair venous return
(Morison et al., 2004; Newton, 2010)
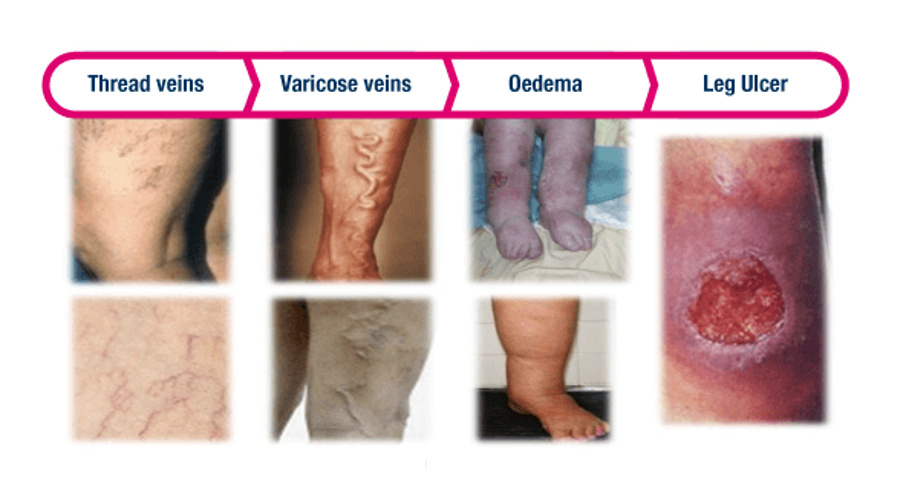
Progression of venous insufficiency