Compression Therapy
Compression therapy is used to manage conditions that are connected with chronic venous insufficiency. It is also used as part of an effective treatment plan for the management of oedema (Wounds UK, 2015).
In general, bandages are most commonly used for the treatment of active VLUs; compression stockings are generally used to prevent recurrence once the ulcer has healed. Compression stockings may also be used in the early stages of chronic venous disease, including thrombotic disease (e.g. deep vein thrombosis), to help prevent disease progression.
Compression bandaging historically has been considered the gold-standard treatment for venous ulceration (Ashby et al., 2014; NICE, 2015). Healing rates of greater than 50% are achievable within 12 weeks (Dowsett, 2012; Vowden & Vowden, 2012). Compression works with exercise to aid drainage of the superficial veins (Dealey, 2005). Compression should be graduated so that the pressure at the ankle is higher than the pressure at the calf.
Principles of Compression Therapy
Treatment is aimed at correcting, as much as possible, the long-term complications of chronic venous insufficiency. Compression therapy systems applied externally to the lower leg increase pressure on the skin and underlying structures to counteract the force of gravity.
This can help to relieve the symptoms in the lower limb by acting on the venous and lymphatic systems to improve removal of fluid (blood and lymph) from the limb.
The most commonly used compression therapy systems come in several forms:
- Bandage components or layers wrapped around the leg (either full leg or below knee)
- Compression hosiery, e.g. compression stockings
- Adjustable Velcro Wrap Devices
(Wounds International, 2013)
How Compression Works
It re-establishes a normal venous flow from the distal regions to the proximal regions. The aim of compression is to optimise the action of the venous pump muscle and direction of venous blood on exertion. It increases the pressure in the tissue under the skin and supports and squeezes the veins, reducing their ability to expand and allowing the valves within the veins to close. This keeps the blood flowing evenly, stopping it from flowing backwards and causing congestion, in turn assisting in the prevention of blood clots.
By improving venous flow, wound healing increases and the risk of infection is reduced. Compression decreases oedema by moving excess fluid back into the blood vessels, which can subsequently reduce pain, improve mobility and improve the patient’s quality of life (Beldon, 2012; Ritchie & Warwick, 2018).
The two main principles at the foundation of how compression therapy works are:
- The creation of an enclosed system that allows internal pressures to be evenly distributed in the leg
- Variation of interface pressures according to limb shape and tension of bandage applied
This will be influenced by bandage/hosiery characteristics and the skill and technique of the person applying the compression.
Key principles of Compression
- To counteract the force of gravity and promote the normal flow of venous blood up the leg
- Acts on the venous and lymphatic systems to improve venous and lymph return and reduce oedema
(Wounds International, 2013)
Compression therapy should be applied with the pressure at the ankle being higher than over the calf and is based upon the original four-layer ‘Charing Cross’ bandage system (Schuren, 2008; Barrett, 2015).
If a compression bandage is applied at the same tension up the lower leg, in theory, a gradual reduction in pressure from ankle to knee will occur automatically (graduated compression). The circumference of the limb is larger at the calf (creating a lower pressure) than at the ankle (higher pressure).
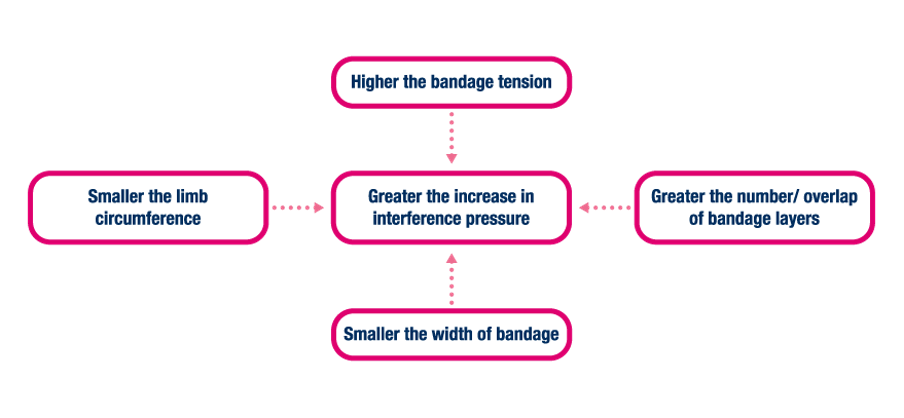
The effect of these variables is characterised by the principle known as Laplace’s Law. In 1805, Pierre-Simon Laplace described a formula that defined the pressures exerted on curved surfaces. Although this law presented a mechanical view of the pressures exerted on curved surfaces, it did not take into consideration the adaptations that occur in humans. The human leg does not have a constant curved configuration, and neither is it solid. In 2003, Thomas adapted Laplace’s law to include the significance of bandage width and number of layers applied to make it more applicable to clinical practice.
The interaction of factors that affect the pressure produced by a compression therapy system — Laplace’s Law Adapted:
P (mmHg) = T (kfg) x N x constant (4620)
C (cm) x W (cm) P = Sub bandage pressure (mmHg) T = Bandage tension (kfg) N = Number of layers C = Circumference of the limb (cm) W =Width of bandage (cm)
The pressures (P) exerted by a compression bandage are directly proportional to the tension (T) and layers (N) but inversely proportional to the circumference (C) of the limb. It is also essential to consider the width (W) of the bandage (BJN, 2015).
This helps us to understand how the interface pressures will vary depending on:
- The limb size at the ankle and calf
- Characteristics of the compression materials used
- The bandage width, the degree of overlap/number of bandage layers and degree of tension applied.
(Wounds International, 2013)
How to choose a compression system
Some key points:
- Patient health status
- Bandage properties - stiffness, pressure, number of layers
- Assessment of the limb
- Wound assessment outcome
- Patient’s lifestyle
- Safety
- Offer patient benefits and improve quality of life
- Easy to use
- Easy to teach or learn
- Clinically effective
- Improve long term patient outcomes
- Cost effective
(Barrett, 2015; Atkins & Tickle, 2016)
There are many different manufacturers of compression bandaging systems. The choice of therapy should be based on a full patient and wound assessment.
Unfortunately, not all patients can tolerate compression therapy. In these cases, a problem-solving approach must be adopted, and the treatment chosen should be appropriate to that individual.
PRECAUTIONS
Compression should only be used following a full holistic assessment and used by trained professionals only.
Compression therapy must not be used on:
- Arterial leg ulcers
- Patients with DVT
- Diabetic patients with advanced disease
- Where the ABPI is less than 0.8 (except when used in a reduced form having been initiated and monitored by a specialist)
(NICE, 2015, 2019)
COMPRESSION HOSIERY
Patients with signs and symptoms of venous or lymphatic insufficiency should be prescribed appropriate hosiery as early as possible to manage the underlying condition and prevent disease progression (Wounds UK, 2015).
Compression hosiery is used to manage conditions associated with chronic venous insufficiency, including post-thrombotic syndrome, varicose veins, venous eczema, lipodermatosclerosis, and swelling in the legs associated with pregnancy (NICE, 2012).