Topic Nine: Topical Negative Pressure Therapy
Topical negative pressure therapy (TNP) is a device which applies a universal negative pressure to a wound to encourage blood flow and faster granulation (Baxendall, 1996). It also removes exudate, reduces bacteria colonisation and reduces odour with the convenience of exudate being removed from the wound (Benbow, 2005).
Mode of Action
The topical negative pressure device assists in wound closure by applying localised negative pressure to the wound bed.
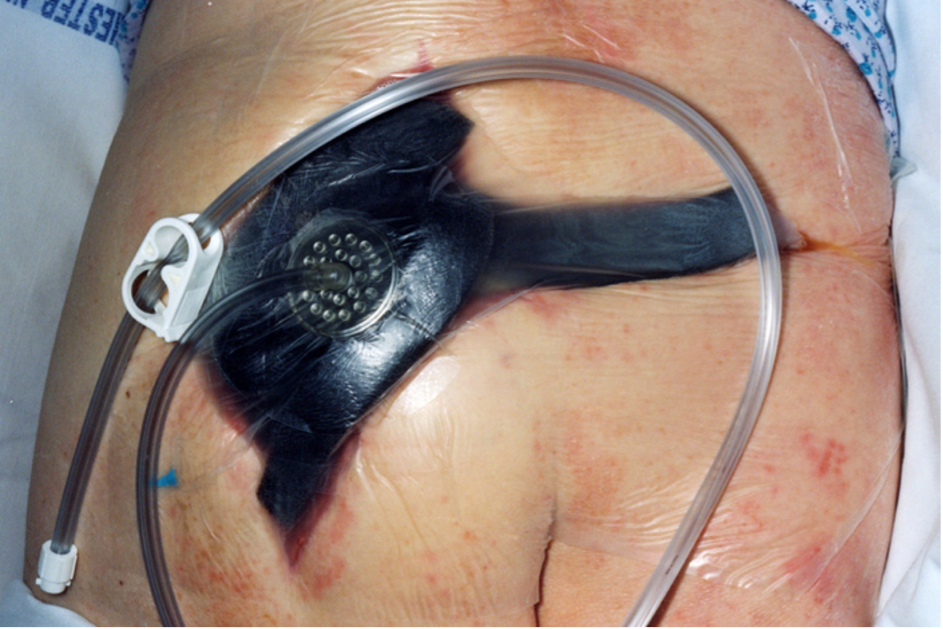
A porous foam dressing or specially designed gauze dressing is positioned in the wound, which is attached to the TNP pump via a tubular plastic drain. The pump controls the degree of negative pressure applied to the wound, and the dressing ensures that the negative pressure is distributed evenly across the wound. An air-tight film dressing is used to secure the porous foam dressing within the wound.
The system creates a hypoxic environment in which aerobic bacteria cannot survive and pulls blood that is rich in growth factors and macrophages into a relatively uncontaminated area (Hampton, 1999; Apelqvist et al., 2017).
The Best Practice Statement (Wounds UK, 2008) states:
‘Gauze-based negative pressure wound TNP therapy has been shown to accelerate debridement, promote angiogenesis, and remove slough and loose necrotic tissue in many wound types´.
Indications for use
Topical negative pressure therapy has been used to manage:
- Acute wounds
- Chronic wounds
- Traumatic wounds
- Sub-acute wounds
- Pressure ulcers
- Diabetic ulcers
- Dehisced surgical wounds
- Skin flaps and grafts
- Infected wounds
Contraindications
Topical negative pressure therapy is contraindicated in the following circumstances:
- Necrotic tissue with eschar
- Malignant wounds
- Untreated osteomyelitis
- Fistulas to organs or body cavities
- Over-exposed arteries or veins
(Wounds UK, 2008)
If haemostasis has been difficult or if a patient has active bleeding or is on anticoagulant therapy, TNP therapy should be used with extreme caution (Benbow, 2008; Apelqvist et al., 2017).
Advantages
- Excellent on heavily exuding wounds
- Assists in the reduction of infection
- Stimulates growth factors
- Accelerates debridement
- Promotes angiogenesis
- Reduces odour
- Accelerates healing and formation of granulation tissue
(Benbow, 2005; Apelqvist et al., 2017)
Disadvantages
- Difficult to apply
- Patient being attached to a machine therefore difficult to move around
- Expensive in both hire of the therapy unit and purchase of the dressings
- Growth of granulation tissue into foam can occur if it is left in place for too long
(Benbow, 2005)
Recent developments have seen the introduction of single-use NPWT for high-risk, post-operative, incision management for more mobile patients.
The introduction of a small, portable and lightweight system could help more patients in the community have the benefits of NPWT without the need to use large systems which may inhibit mobility and day-to-day activity’ (Timmons & Russell, 2012). This method is also well accepted by patients and clinicians despite limited scientific proof of its usefulness. Therefore, more scientific research is required.
To conclude, topical negative pressure therapy can be very effective and convenient, and removes excess exudate and odour. It can also be cost-effective as it can reduce the overall time taken for a wound to heal (Benbow et al., 2007).
This module has looked at the evidence surrounding wound care and at the commonly used dressings and wound management products. This is not an exhaustive list of wound management options available to practitioners, and therefore, you may wish to conduct further research into the products available. Please see the recommended further reading section.
The information given here is a general guide only and must not replace clinical judgement. Individuals are advised to make their own further enquiries to manufacturers regarding specific treatments or products.
Specialist advice can also be obtained from the Tissue Viability Service provided by individual hospital and community trusts or from other clinical specialists.
When you are ready, please complete the following “Test Your Knowledge” section…