Topic Six: Silver Dressings
Silver has been used in wound care since the 17th Century when silver nitrate was used to treat proud flesh and sores. Over the years, silver has been used in a variety of different ways, from inserting solid silver into wounds or as silver salts, creams and ointments (Hedger, 2015). There has been a recent resurgence of interest in the use of silver for its antibacterial properties in wound care as a result of increasing problems associated with antibiotic resistance (White, 2001). Silver sulphadiazine has been very successful in controlling burn wound infections (Fakhry, Alexander & Smith, 1995).
There is no current robust clinical or cost-effective evidence to support the use of antimicrobial dressings (for example, silver, iodine, or honey) over non-medicated dressings for preventing or treating chronic wounds. Indiscriminate use should be discouraged because of concerns over bacterial resistance and toxicity.
Antimicrobial dressings may be considered to help reduce bacterial numbers in wounds but should be avoided unless the wound is infected or there is a clinical risk of the wound becoming infected (NICE, 2015).
Wound infections present problems, including delayed healing. Almost all skin infections are sensitive to silver as an antibiotic, and there is increasing evidence that shows that sustained silver release technology is well suited in treating difficult-to-heal wounds (Lansdown, 2002).
Silver is found in dressings in several forms:
- Elemental silver – e.g. silver metal, nanocrystalline silver
- An inorganic compound – e.g. silver oxide, silver phosphate, silver chloride, silver sulfate, silver-calcium-sodium phosphate, silver zirconium compound, SSD
- An organic complex – e.g. silver-zinc allantoinate, silver alginate, silver carboxymethylcellulose
(International Consensus: Silver, 2012)
The silver component of dressings may appear:
- As a coating – on one or both external surfaces of the dressing (elemental or nanocrystalline silver)
- Within the structure of the dressing – either as a coating on dressing materials (elemental or compound silver), within the spaces of the dressing materials (elemental or compound silver), or as a compound that forms part of the dressing structure (e.g. silver alginate)
- As a combination of these
(International Consensus: Silver, 2012)
The continual development of wound care dressings that contain silver has altered how silver can be applied to a wound. These dressings can provide a sustained delivery of silver, which, along with other properties such as absorbency, means that a moist wound environment can be maintained, and the dressing does not need to be changed as frequently. Silver is now available in a variety of forms for wounds and can be found added to many types of commonly used dressings. Silver comes in different presentations, such as tulle, paste, foam and alginates (Hedger, 2015).
Mode of Action
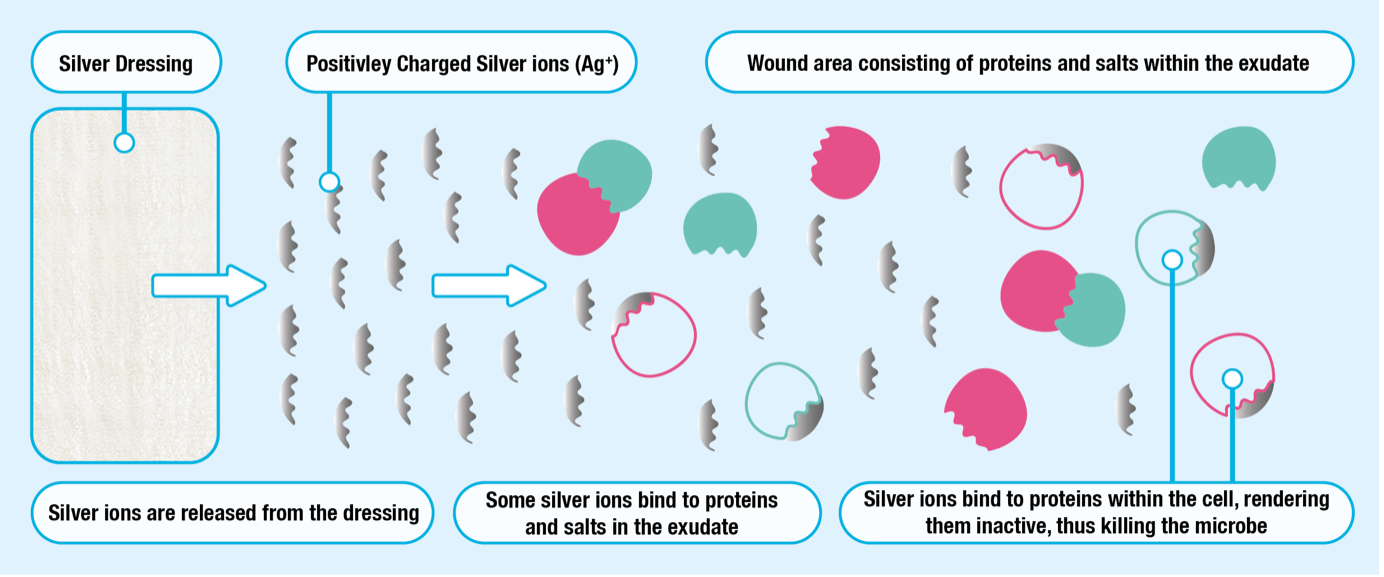
Silver, in its metallic form, does not readily interact with the tissues of the human body and is unable to kill bacteria. To become an effective bactericidal silver, atoms must lose an electron and become positively charged silver ions. Elemental silver ionises in the air but ionises more readily when exposed to an aqueous environment such as wound exudate.
Silver ions are highly reactive and affect multiple sites within bacterial cells when the silver ions bind to them. This ultimately results in the bacterial cell death. They bind to bacterial cell membranes, causing disruption of the bacterial cell wall and cell leakage. Silver ions are active against a broad range of bacteria, fungi and viruses, including many antibiotic-resistant bacteria, such as Meticillin-Resistant Staphylococcus Aureus (MRSA) and Vancomycin-Resistant Enterococci (VRE).
(International Consensus, Silver 2012; Hedger, 2015)
Silver wields its action in one of two ways:
- On contact with wound exudate, silver ions are released into the wound bed and kill the bacteria at the wound bed.
- Exudate is absorbed into the dressing, where the silver kills the bacteria within the dressing.
(Hedger, 2015)
It is important for clinicians to know the mode of action of the dressing they are using, as some require moistening with water (not saline) to enable the release of silver ions, while others can be applied directly (Hedger, 2015).
Studies of the effects of silver dressings on experimental models of biofilms (Box 3) have suggested that silver may reduce bacterial adhesion and destabilise the biofilm matrix, as well as kill bacteria within the matrix and increase the susceptibility of bacteria to antibiotics.
Silver, in its metallic form, does not readily interact with tissues of the human body. However, in the presence of moisture, body fluids and wound exudate, silver ionises to release Ag+ ions. The concentration of the Ag+ ions released is disproportional to the antiseptic efficacy of the product (White & Cutting, 2006).
In 2012, the International Consensus document on silver stated:
The total amount of silver in dressings varies considerably. In a wound environment, the interaction of silver ions with wound components, such as chloride ions and proteins, means that the amount of silver delivered to a wound does not correlate with the amount of silver contained in the dressing. Although in some laboratory experiments, very low concentrations, e.g. one part per million (1ppm) of silver ions or less, have been shown to be effective against bacteria, it is unclear how silver content and availability measured in experimental settings relate to clinical performance.
Sustained silver release dressings in wound management
The aim of silver-containing dressings is primarily to continuously release small amounts of antimicrobial silver into the wound to inhibit the growth of bacteria.
When selecting a silver dressing, the following should be taken into consideration:
- Does it deliver silver in a sustained therapeutic way into the wound?
- Will it absorb exudate?
- Does it have odour control?
- Is it comfortable and easy to apply?
- Is it comfortable and acceptable for the patient?
- Is it cost-effective?
- Is there an infection in the wound?
(White, 2001; Wound Care Today, 2017)
There are many silver-release dressings currently available that vary in their composition and clinical indications for use. However, they all exhibit the following ‘main’ features:
- Release ‘active’ silver ions in a controlled way during the stages of wound healing (up to seven days)
- Exhibit broad-spectrum anti-bacterial activity in the wound bed
- Manage wound exudate, odour and pain
- Easy to apply, conformable and atraumatic removal
- Cost-effective
- Benefit wound healing
(Lansdown, 2002; Wound Care Today, 2017)
Indications for use
Silver dressings are indicated for use on infected wounds. Silver-containing dressings can potentially be expensive. Therefore, they should not be used on wounds that are not infected or not at risk of becoming infected.
NICE BNF 2018 states:
‘Antimicrobial dressings containing silver should be used only when infection is suspected as a result of clinical signs or symptoms’.
The Best Practice Statement for the use of topical antiseptic or antimicrobial agents in wound management (Wounds UK, 2011) states:
‘It is important to avoid using antimicrobial agents on wounds where infections are not present’.
Prophylactic Use
Antimicrobial dressings, such as silver, can be used as an impediment to microorganisms present in wounds that are at a high risk of infection or re-infection. Examples of these wounds include:
- Burns
- Surgical wounds - due to the patient’s high risk of infection, type and location of surgery
- Pressure ulcers near the anus
- Wounds with exposed bone
- Wounds in patients who are immunocompromised, have poor circulation, unstable diabetes or neoplastic disease
(International Consensus: Silver, 2012)
Contraindications
- Silver dressings are contraindicated in hepatic and renal failure patients, pregnancy and lactation, and in newborns
- Silver dressings are not effective in dry wounds
- Silver dressings cannot prevent infection and are not always the most cost-effective dressing when used prophylactically
- Do not use if sensitivity to silver occurs; this can cause pain and burning sensation
- Do not use long term without specialist advice and support
- Do not use during radiotherapy or magnetic resonance imaging scanning
(Hedger, 2015)
NB - Not all silver dressings will have these contraindications, always refer to the manufacturer’s instructions for use.
Some patients may produce a hypersensitivity reaction to product ingredients, such as silver (Vuolo, 2009). These dressings should only be used if clinically infected or if the wound is at risk of becoming infected.
When using a silver-containing dressing, the clinician must read the indications for use leaflet to ensure that it is being used appropriately and that the product is being used within licence. Clinicians should also ensure that they are following the wound care formulary of the local trust.
To conclude, new dressings containing silver permit a controlled release of silver ions for up to seven days, and they have become very popular as an effective means of managing infected and chronic wounds.
For further information, visit: NICE