Topic Three: Foam Dressings
Composition & Properties
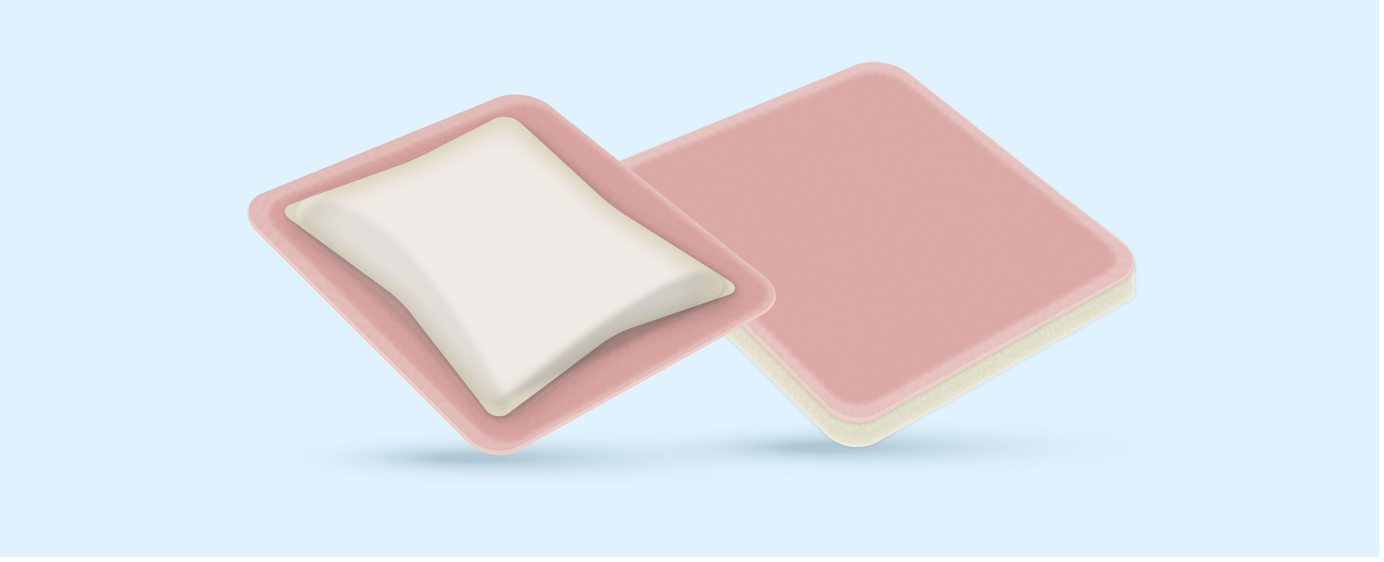
Foams usually consist of an absorbent polyurethane foam, which is sometimes combined with other components. Foams are able to provide a moist healing environment and they are usually available in flat sheets (with or without an adhesive border) or as a cavity dressing.
Foam dressings, with or without plastic film backing, containing hydrophilic polyurethane foam are suitable for all types of wounds except for dry wounds. These dressing types vary in their ability to absorb exudate; some are indicated for lightly to moderately exuding wounds and others have a greater fluid handling capacity. Foam dressings can also be used to provide a protective cushion for fragile skin (British National Formulary, 2015, 2020).
Foams can be applied directly onto the wound as a primary dressing or, in conjunction with other wound management products, as a secondary dressing. Some foam dressings have a vapour-permeable back sheet, which allows the passage of moisture out of the dressing. This helps to reduce the build-up of exudate and, thus, prevents the risk of skin and wound maceration underneath the dressing.
Foam dressings should not be held in place with adhesive film dressings as this will reduce the moisture vapour transfer rate (MVTR) of the dressing and consequently reduce the dressing’s exudate handling properties. Non-adhesive foam dressings should be fixed in place with a suitable tape to ensure the dressing remains centrally located. Non-adhesive foams should be chosen for the treatment of patients with a known adhesive sensitivity, fragile skin and for wounds that will require frequent re-dressing in order to protect the periwound area from adhesives.
The time at which the dressing should be changed will depend on the volume of wound exudate being produced and the product that has been selected. Therefore the manufacturer’s instructions should be followed.
Silicone Foams
Many foam dressings use silicone as an alternative to acrylic adhesive. Some foams now incorporate a soft silicone wound contact layer. This layer forms a gentle bond between the wound surface and the dressing. It ensures that fluid is absorbed by the dressing and does not linger on the surface of the skin. In clinical studies, such dressings have been shown to wick fluid vertically with no lateral movement of exudate from the wound onto the surrounding skin (Meuleneire 2013).
They are particularly suitable for patients:
- With fragile skin, including young children and the elderly
- Where the patient experiences pain at dressing changes
- Needing protection for at-risk periwound skin
(Meuleneire, 2013)
It has been shown that when removed from the skin, soft silicone dressings do not cause trauma to the wound or periwound skin (Rippon, 2007). They have been described as ‘atraumatic’ for this reason.
It is important to note that not all silicone foam dressings can be described as atraumatic.
Foam dressings that just incorporate silicone as the adhesive border cannot necessarily be described this way. This is because they may not have a wound contact layer, or the contact layer may not be soft silicone. This means the dressing could potentially adhere to the wound bed.
Foam dressings feature the following general performance properties and attributes:
- Help maintain moist wound environment
- Protect wound and periwound area against trauma
- Easy to apply and remove
- May be used under compression
- Conformable
- Can be used with topical agents or enzymatic debriders
- Non adherent
- Allows for atraumatic removal
- Semi permeable
- Can stay in place for up to seven days depending on the amount of wound exudate
(Wound Source, 2017)
Indications for use
Foam dressings are indicated for flat or cavity wounds with a varying amount of exudate, depending on the product and are recommended for use in exuding sloughy and granulating wounds (Morris, 2006). It has been suggested that some foam dressings may be useful in the treatment of over granulation (Vuolo, 2010).
Foams are not indicated for use on dry necrotic wounds except in conjunction with a suitable debriding agent.